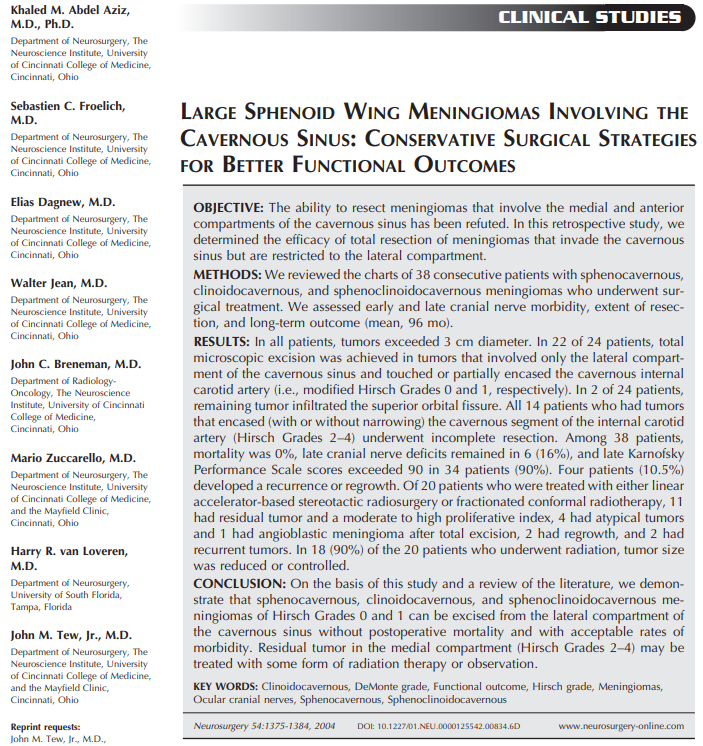
涉及海绵窦的大型蝶骨翼脑膜瘤:保守的手术策略以获得更好的功能结果(Large sphenoid wing meningiomas involving the cavernous sinus: conservative surgical strategies for better functional outcomes)
英文摘要:
OBJECTIVE: The ability to resect meningiomas that involve the medial and anterior compartments of the cavernous sinus has been refuted. In this retrospective study, we determined the efficacy of total resection of meningiomas that invade the cavernous sinus but are restricted to the lateral compartment.
METHODS: We reviewed the charts of 38 consecutive patients with sphenocavernous,clinoidocavernous,and sphenoclinoidocavernous meningiomas who underwent surgical treatment. We assessed early and late cranial nerve morbidity, extent of resection, and long-term outcome (mean, 96 mo).
RESULTS: In all patients, tumors exceeded 3 cm diameter. In 22 of 24 patients, total microscopic excision was achieved in tumors that involved only the lateral compartment of the cavernous sinus and touched or partially encased the cavernous internal carotid artery (i.e., modified Hirsch Grades 0 and 1, respectively). In 2 of 24 patients, remaining tumor infiltrated the superior orbital fissure. All 14 patients who had tumors that encased (with or without narrowing) the cavernous segment of the internal carotid artery (Hirsch Grades 2-4) underwent incomplete resection. Among 38 patients, mortality was 0%, late cranial nerve deficits remained in 6 (16%), and late Karnofsky Performance Scale scores exceeded 90 in 34 patients (90%). Four patients (10.5%) developed a recurrence or regrowth. Of 20 patients who were treated with either linear accelerator-based stereotactic radiosurgery or fractionated conformal radiotherapy, 11 had residual tumor and a moderate to high proliferative index, 4 had atypical tumors and 1 had angioblastic meningioma after total excision, 2 had regrowth, and 2 had recurrent tumors. In 18 (90%) of the 20 patients who underwent radiation, tumor size was reduced or controlled.
CONCLUSION: On the basis of this study and a review of the literature, we demonstrate that sphenocavernous, clinoidocavernous, and sphenoclinoidocavernous meningiomas of Hirsch Grades 0 and 1 can be excised from the lateral compartment of the cavernous sinus without postoperative mortality and with acceptable rates of morbidity. Residual tumor in the medial compartment (Hirsch Grades 2-4) may be treated with some form of radiation therapy or observation.
中文摘要:
目的:脑膜瘤累及海绵窦内、前室的切除能力已被否定。在这项回顾性研究中,我们确定了侵袭海绵窦但局限于侧腔室的脑膜瘤全切除的疗效。
方法:我们回顾了38例接受手术治疗的海绵窦、斜海绵窦和海绵窦脑膜瘤的病例。我们评估了早期和晚期脑神经病变、切除范围和长期预后(平均96个月)。
结果:全部患者肿瘤直径均超过3cm。在24例患者中,有22例肿瘤仅累及海绵窦外侧腔室,并触及或部分包裹颈内动脉,即颈动脉(分别为0级和1级)。24例中有2例肿瘤浸润眶上裂。全部14例颈内动脉海绵样节段(Hirsch分级2-4)包绕(或不包绕)的肿瘤均行不完全切除。38例患者死亡率为0%,晚期脑神经缺损6例(16%),晚期Karnofsky功能评分超过90分34例(90%)。4例(10.5%)出现复发或再生长。采用直线加速器立体定向放射治疗或分割适形放射治疗的20例患者中,11例有残留肿瘤,增殖指数中等高,4例为非典型肿瘤,1例为全切除后的血管成细胞脑膜瘤,2例再生,2例复发。在20例接受放射治疗的患者中,有18例(90%)的肿瘤缩小或得到控制。
结论:在此研究的基础上,回顾文献,我们证明海绵窦,斜海绵窦,和斜海绵窦脑膜瘤的侧腔室可切除,海绵窦无术后死亡,可接受的发病率。内腔室残留的肿瘤(Hirsch分级2-4级)可能是用某种放射疗法或观察治疗的。
1910年,Frotscher和Becker(21)在尸检中一次报告了一例蝶窦型脑膜瘤;后来它被命名为文森特的海绵窦角的囊状内皮瘤。1938年,Cushing和Eisenhardt将蝶骨嵴脑膜瘤分为深部内型或斜坡型;中间或腋下;以及外翼的。我们认为翼点脑膜瘤是一种以明显的骨质增生为特征的凸性脑膜瘤。中、深部蝶骨嵴脑膜瘤可通过在常规翼点入路的基础上增加眼眶或眶颧骨截骨术而转变为倒置凸性脑膜瘤。内蝶骨翼和斜窦脑膜瘤是一项艰巨的手术挑战,当它们延伸到海绵窦并变成斜窦、蝶窦时。
我们治疗海绵窦脑膜瘤的目的是提高患者的功能预后。我们认为,神经外科医生应该能够切除海绵窦侧腔(Hirsch级别 0 - 1)的肿瘤部分,而不造成术后死亡,并且具有可接受的眼部CN发病率。根据细胞异型性、增殖指数、患者年龄和临床情况,对中室残留肿瘤(Hirsch级别 2 - 4)应行观察或放疗。采用这些保守的手术方法,我们获得了16%的发病率,6%的复发率,8%的再生率。
该研究主要人员之一为INC国际神经外科医生集团旗下组织国际神经外科顾问团(WANG)成员、国际神经外联合会(WFNS)颅底手术委员会主席(2013年至今)Sebastien Froelich教授。
- 文章标题:涉及海绵窦的大型蝶骨翼脑膜瘤:保守的手术策略以获得更好的功能结果
- 更新时间:2019-12-02 18:07:25

 400-029-0925
400-029-0925