英文原文:
Gardner and colleagues have described their series of 16 patients who underwent an endoscopic, expanded endonasal approach (EEA) for craniopharyngioma between 1999 and 2006. The primary outcomes of their study included the following: endocrine and ophthalmological results, ex- tent of resection, and complications. The majority of their patients underwent planned complete resection. In these patients, 73% (8 of 11) had a gross-total resection without recurrence during a mean follow-up of 34 months. No patient in the series experienced visual worsening. The postoperative rate of permanent diabetes insipidus (DI) was 8%. Cerebrospinal fluid (CSF) leaks were documented in 58% of patients. In 1 patient, a stroke occurred from a perforating vessel from a posterior cerebral artery injury.
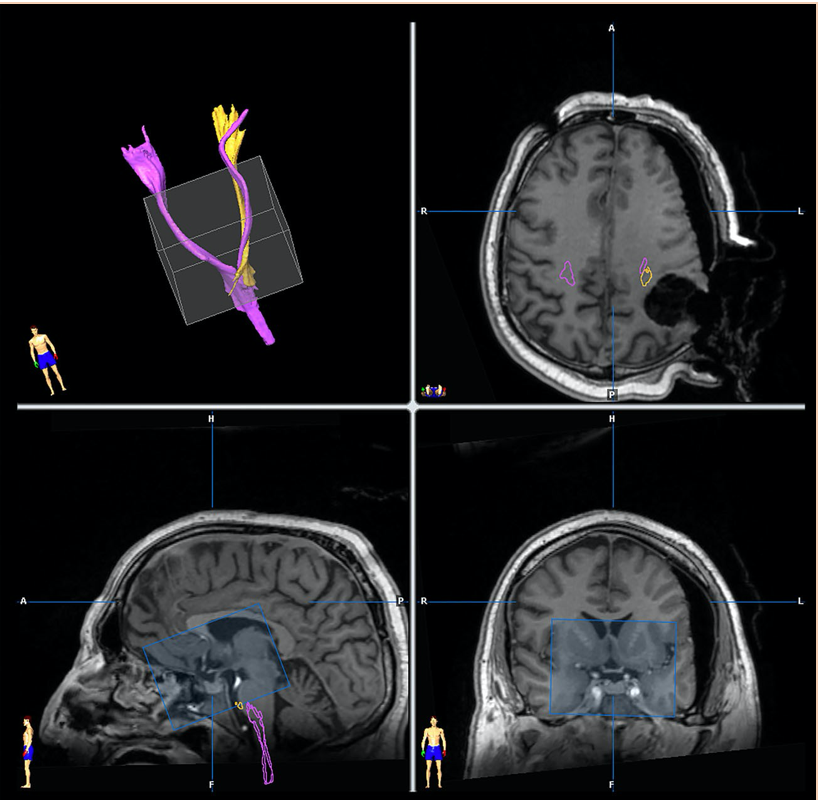
Of interest here is the classification of craniopharyngio- mas into a system that is best appreciated by the endoscopic, endonasal neurosurgeon: Type I, preinfundibular; Type II, transinfundibular; and Type III, retroinfundibular. In the- ory, this is an attractive classification system. In practice, however, there will be instances in which the craniopharyngiomas are either too large and the stalk obscured, or the MR images will be inadequate to fully ascertain the location of the tumor with respect to the infundibulum. I would like to commend the authors on their willingness to tackle some of the more difficult types of craniopharyngiomas (for example, the Type IIIa and IIIb lesions) through an EEA. Years ago, I would have thought such an approach to the “retrochiasmatic” craniopharyngioma would have been impossible. Now, with the advent of the techniques that have been uniquely shared by the minimally invasive neurosurgeon and otolaryngologist and which are expounded on in this study, craniopharyngiomas of all types can be the target of EEA.
As with all new techniques that come forward for analysis when compared with established, conventional ones, a critical review of the complications must be undertaken. Here, it is clear that EEA for craniopharyngioma is well tol- erated, and the vast majority of patients do well after tumor resection. Endocrine and ophthalmological functions were reasonably well preserved and/or maintained. The one area, of course, where greater strides will need to be taken and where improvements in technique will be mandatory is with the rate of CSF leakage. However, it sounds as though the authors are well on their way to improving their out- comes with CSF leaks by using vascularized mucosal flaps together with local reinforcement of the sellar floor.
This report by Gardner and associates is more than a technical note, but is not yet quite at the level of the larger published series on craniopharyngioma1-4 in which more patients with craniopharyngioma have been studied and followed, in some instances, for longer periods of time. In all series, however, including the present one, recurrences of craniopharyngioma are a fact of life. The rate of recurrence may be as high as 40% in some series. The treatment of the recurrent craniopharyngioma is a vexing problem, and one wonders whether patients who were first treated using the EEA would again be candidates for a repeated procedure using this approach.
The EEA described here was performed in adults. As craniopharyngiomas commonly occur in children, it would be interesting to use this approach in the child with a craniopharyngioma. In this regard, the limitations would likely be similar to those observed with the transsphenoidal approach in this age group: small nares, nonpneumatized sella, and smaller midline corridor between the carotid arteries.
Finally, as the authors expand their series and gather more patients for analysis, I exhort them to analyze the effects of EEA on the neuropsychology of their patients. It is here that I suspect that EEA may be a beneficial approach over craniotomy and subfrontal or pterional approaches to craniopharyngioma.
中文翻译:
Gardner和他的同事描述了他们在1999年至2006年间对16例颅咽管瘤患者进行的内镜下扩大鼻道入路(EEA)治疗。他们的研究的主要结果包括:内分泌和眼科结果,切除前,和并发症。他们的大多数病人都接受了计划中的全切除手术。在这些患者中,73%(11例中的8例)在平均34个月的随访中进行了总切除,没有复发。在这个系列中没有病人出现视觉恶化。术后长期性尿崩症(DI)发生率为8%。58%的患者有脑脊液(CSF)渗漏的记录。1例发生脑后动脉损伤穿孔血管卒中。
我们感兴趣的是颅咽- mas系统的分类它是由内窥镜,鼻内神经外科医生较能理解的:I型,漏斗前;II型,transinfundibular;III型,漏斗后。在理论上,这是一个有吸引力的分类系统。然而,在实践中,有时颅咽管瘤太大,茎部模糊不清,或者MR图像不足以完全确定肿瘤相对于漏斗部的位置。我想赞扬作者们愿意通过EEA来处理一些较困难类型的颅咽管瘤(例如,IIIa型和IIIb型病变)。几年前,我认为这种治疗“交叉后”颅咽管瘤的方法是不可能的。现在,随着微创神经外科医生和耳鼻喉科医生所技术的出现,以及本研究中所阐述的技术,各种类型的颅咽管瘤都可以成为EEA的目标。
与全部新出现的分析技术相比,现有的,传统的,一个关键的审查并发症需进行。可见,颅咽管瘤的EEA治疗进展良好,多数患者肿瘤切除后恢复良好。内分泌和眼科功能得到合理的保存和/或维持。当然,有一个领域需要更大的进步,技术上的改进是需的,那就是CSF的泄漏率。然而,这听起来好像作者们在好转他们的方法上做得很好--通过使用带血管蒂的粘膜瓣和颅底的局部加固来好转CSF泄漏。
Gardner和同事的这篇报告不仅仅是一个技术说明,但还没有达到颅咽管瘤1 - 4系列报道的水平,在该系列报道中,对更多的颅咽管瘤患者进行了研究,并在某些情况下进行了更长时间的随访。然而,在全部的病例中,包括目前的病例,颅咽管瘤的复发是不可避免的。某些系列的复发率可能高达40%。复发性颅咽管瘤的治疗是一个令人烦恼的问题,人们想知道一次使用EEA治疗的患者是否会再次成为使用这种方法重复手术的候选人。
这里描述的EEA是在成人中进行的。由于颅咽管瘤通常发生在儿童中,因此对颅咽管瘤儿童采用这种方法将是很有趣的。在这方面,局限性可能与经蝶窦入路在这个年龄组中观察到的局限性类似:鼻孔小、非气化蝶鞍、颈动脉间更小的中线走廊。
较后,随着作者扩大他们的系列并收集更多的患者进行分析,我建议他们分析EEA对患者神经心理的影响。在这里,我怀疑相对于开颅术和额下入路或翼点入路,EEA可能是一种治疗颅咽管瘤的有益方法。
该论文作者为INC国际神经外科医生集团旗下国际神经外科顾问团(WANG)成员、国际神经外科学院院长(2011-2014)James T. Rutka教授。
资料来源:https://sci-hub.se/https://www.ncbi.nlm.nih.gov/pubmed/18590425
- 文章标题:颅咽管瘤的经鼻切除术(Endonasal resection of craniopharyngiomas)
- 更新时间:2019-12-09 17:24:59

 400-029-0925
400-029-0925