脑干肿瘤占成人全部颅内肿瘤的1.5%至2.5%,而占儿童肿瘤的10%至20%。这些肿瘤在成人中不常见,因此,更多的临床研究已经在患有脑干肿瘤的儿童中进行,特别是脑干胶质瘤,因为他们在这类患者群体中更常见。患有脑干胶质瘤的成人的中位生存期为5到7年,比儿童要长。由于手术预后差及手术致残率高,脑干和颈髓交界区内的肿瘤在现代神经外科之前被认为不能手术。Pool在1968年记录了一例位于脑导水管区域的脑干肿瘤的手术切除。这个报告的病例带来了对治疗脑干病变的进一步研究和外科技术的发展。
脑干肿瘤的分类
脑干肿瘤较早的分类方案是基于CT图像和手术观察。随着磁共振成像(MRI)技术的出现,对此类肿瘤的手术决策过程起重要作用的两个关键性成像特征可能是:精确的解剖位置和局灶性与弥漫性的形态。因此,基于这些影像学特征而非肿瘤组织学的不同亚型来指导手术范式。一般将肿瘤分为局灶性或弥漫性生长模式,而更复杂的分类进一步将肿瘤细分为脑干内位置、有无外生性成分、有无脑积水或出血。事实上,诊断往往可以通过术前影像来做出,从而指导是否手术。一般来说,与弥漫性生长模式的肿瘤相比,局灶性生长模式的肿瘤被认为更适合手术切除。
局灶型脑干胶质瘤
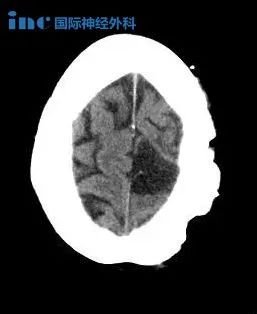
这一类肿瘤可表现为实体瘤或囊性肿瘤(图13-1),类似于小儿小脑星形细胞瘤。症状通常不明显和局限于肿瘤附近的结构。如果影像学表现为局灶性病变,但其临床过程与弥漫性桥脑胶质瘤一致,那么就会表现为高度恶性的肿瘤。出于这个原因,仔细获取临床病史是必要的。此外,大多数颈髓神经胶质瘤是低级别的非浸润性肿瘤,其生长通常受到皮质脊髓束和内侧丘系白质的限制。
虽然肿瘤通常位于延髓,表现为后组颅神经病变(吸入、吞咽困难、呼吸暂停、舌肌无力/萎缩),但是也可能发生在脑桥(引起面神经或听力以及皮质脊髓束功能障碍)或中脑(引起动眼神经功能障碍或脑积水)。
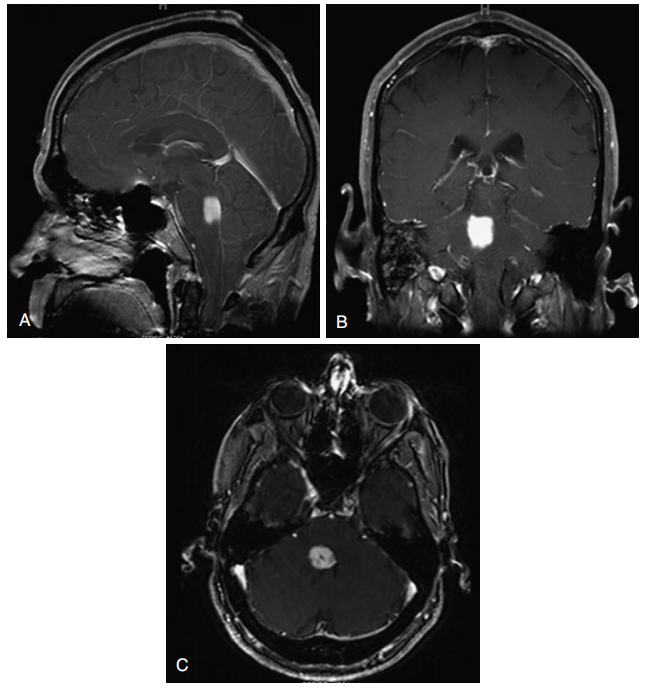
图13-1局灶性桥脑胶质瘤。A,矢状面MRI显示脑桥强化肿块。B,造影后冠状核磁共振成像。C,对比后轴向MRI。
Focal pontine glioma.A, Post-contrast sagittal MRI demonstrates an enhancing mass in the pons. B, Post-contrast coronal MRI. C, Post-contrast axial MRI.
外生型胶质瘤
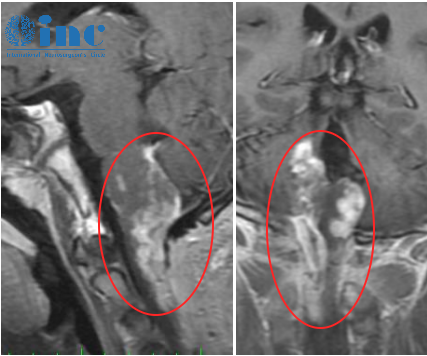
具有外生生长成分的局灶型脑干胶质瘤通常是低级别的,界限清楚(图13-2)。它们通常是生长到四脑室的背侧外生肿瘤或外生生长到大池和四脑室的颈髓肿瘤。值得一提的是,除了局灶型肿瘤外,一些弥漫型肿瘤可能引起四脑室、桥小脑角、前脑池和其他脑池的膨出。
Focal brain stem tumors with an exophytically growing component are usually low-grade and well circumscribed (Fig. 13-2). They are typically dorsally exophytic tumors growing into the fourth ventricle or cervicomedullary tumors with exophytic growth into the cisterna magna and
fourth ventricle . It should be mentioned that, in addition to focal tumors, some diffuse tumors may cause bulging into the fourth ventricle, cerebellopontine angle, and prepontine and other cisterns.
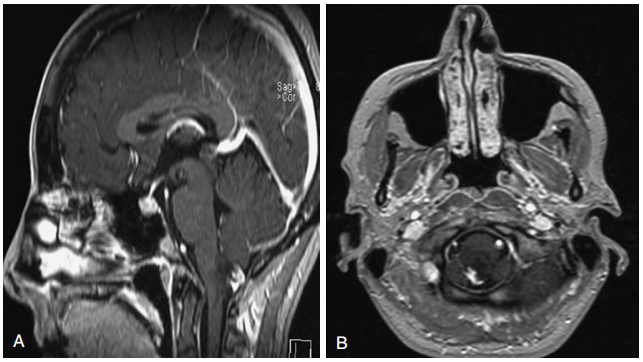
图13-2背侧外生性颈髓胶质瘤。A、 矢状位磁共振造影后显示一低信号病灶,在尾侧部分有强化。
B、轴位磁共振造影后。
Dorsal exophytic cervicomedullary glioma. A, Post-contrast sagittal MRI demonstrates a hypointense lesion with enhancement in the posteriocaudal part.
B, Post-contrast axial MRI.
弥漫型脑干胶质瘤
也被称为弥漫型桥脑胶质瘤(DPG),这种肿瘤无论其组织病理学如何,必然进入恶性进展。超过三分之二的脑干胶质瘤是DPGs,并且它们通常可以通过MRI影像做出诊断。肿瘤以弥漫扩展的脑桥为中心,延伸入延髓和/或中脑,而无局灶性或外生性部分。
DPGs通常可见基底动脉的侵蚀。此肿瘤患者通常表现为双侧进展性颅神经病变,其次是皮质脊髓束功能障碍和脑积水。通常不建议活检,因为活检有导致额外神经功能缺损的。此外,活检不会影响病人行姑息性化疗和放疗;预后差。
弥漫性脑干肿瘤在T1加权和T2加权MR图像上分别表现为低至等信号和高信号(图13-4)。对比剂注射后有不同程度的增强,这些肿瘤的对比剂增强可能提示恶性变性。此外,肿瘤边界无法在MRI上描绘,脑干通常增大和变形。
Diffuse brain stem tumors appear hypo- to iso-intense and hyper-intense on T1-weighted and T2-weighted MR images, respectively (Fig. 13-4). There is variable enhancement with contrast administration, and contrast enhancement in these tumors may be indicative of malignant degeneration. Moreover, the tumor boundaries are not able to be delineated on MRI, and the brain stem is typically enlarged and deformed.

图13-4弥漫性桥脑胶质瘤。A、 T2加权矢状位MRI显示桥脑高信号肿块。
B、 对比后矢状位T1加权MRI显示低信号、无强化的脑桥肿块。
C、 低信号,无强化的桥体肿块在轴向T1加权磁共振造影后。D、 T2加权轴位MRI显示桥脑高信号肿块。
Diffuse pontine glioma. A, T2-weighted sagittal MRI demonstrating hyperintense mass in the pons.
B, Hypointense, nonenhancing pontine mass on postcontrast sagittal T1-weighted MRI.
C, Hypointense, nonenhancing pontine mass on post-contrast axial T1-weighted MRI. D,T2-weighted axial MRI demonstrating hyperintense pontine mass.
手术适应证
如上所述,脑干胶质瘤分为两大类:弥漫型和局限型。弥漫型胶质瘤通常是非手术病变。然而在少见的情况下,当影像学诊断有问题时可行活检。局灶型脑干胶质瘤可以手术切除,这通常是优选的治疗方法。背侧中脑肿瘤,如顶盖型胶质瘤是良性的,通常不需要手术切除,如果MRI上显示肿瘤进展的情况下可以进行手术。
脑积水的治疗可在病变切除之前或切除当时进行;术前临时的脑脊液(CSF)分流(三脑室底造瘘术)有助于好转症状和防止术后脑脊液经手术部位渗漏。梗阻性肿块切除后,患者不需要长期性脑脊液分流。
影像学上边界明确的进展性局限型、背侧外生型和颈髓型胶质瘤引起症状的轴外成份可行次全切除。脑干内的神经胶质瘤的切除有风险,不建议切除。局限型良性胶质瘤是个例外,如毛细胞型星形细胞瘤;应审慎考虑手术。
成人脑干胶质瘤顺利全切后10年+没有复发案例报告3则
下文主要报导德国巴特朗菲教授全切成人脑干胶质瘤3例及术后长期随访的病例,该良好的临床效果发表于2020年的脑干肿瘤手术经典专著《Surgery of the Brainstem》中13章Adult Brainstem Gliomas(成人脑干胶质瘤)。
案例1:较大脑干毛细胞星形细胞瘤全切10年没有复发
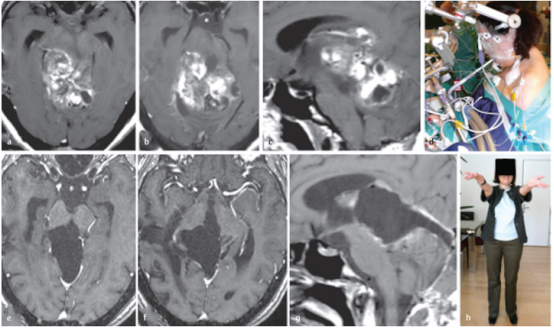
简要病史:28岁女性,有进行性步态共济失调和轻微复视。在德国INI就诊的四年前,在本国医院被诊断出中脑顶盖肿瘤,接受了两次外科手术检查,活检诊断出毛细胞星形细胞瘤。随着肿瘤继续长大,建议患者在其他地方接受放疗,然后用替莫唑胺进行化疗,为期12个月,然而治疗均未达到合适的肿瘤控制。
术前:术前轴位(a,b)和矢状面(c)MRI显示,较大肿瘤,从中脑两侧延伸到丘脑、脑桥和小脑。
术中:半坐位,广泛性肿瘤切除术
术后:轴位(e,f)和矢状位(g)T1加权增强MRI检查显示,外生毛细胞星形细胞瘤被成功切除。病人没有出现额外的神经功能缺损,随后的病程平安无事。h,显示在根治性肿瘤切除术后10年的随访中,患者的病情持续良好,没有复发。
This 28-year-old woman had progressive gait ataxia and slight diplopia. A midbrain tectal tumor was diagnosed in her home country 4 years before her presentation to our clinic. The patient underwent 2 surgical explorations in other hospitals, and each time no more than a tumor biopsy was undertaken. Histopathologically, a pilocytic astrocytoma was diagnosed. As the tumor continued proliferating, the patient was advised elsewhere to undergo radiotherapy and thereafter chemotherapy with temozolomide for a period of 12 months. When the patient presented to our institute for the first time, the tumor had reached a very large size, extending from the midbrain into the thalamus, pons, and cerebellum bilaterally as shown on preoperative axial (a,b) and sagittal (c) magnetic resonance images (MRIs). As none of the previous therapies achieved efficient tumor control, we offered the patient extensive tumor resection. (d) She agreed and underwent the procedure in the semisitting position. Complete removal of this exophytic pilocytic astrocytoma World Health Organization grade I tumor was successful as documented on postoperative axial (e,f) and sagittal (g) T1-weighted contrast-enhanced MRIs. The patient experienced no additional neurologic deficits, and her subsequent course was uneventful. (h) At 10-year follow-up after radical tumor removal, the patient continued to do well and remained recurrence-free.
案例2:背侧外生型中脑毛细胞星形细胞瘤全切11年没有复发
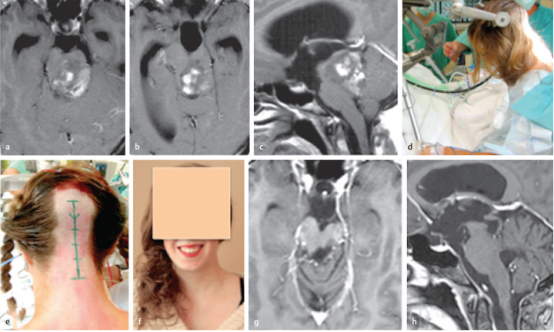
简要病史:20岁女孩由于背侧外生的中脑肿瘤引起的梗阻性脑积水而较度头痛。
术前:术前的轴位(a,b)和矢状位(c)对比增强MRI提示高级别肿瘤累及中脑和上脑桥。然而,由于患者没有神经功能缺损,肿瘤恶性程度似乎不太可能,并与患者及其家人讨论了低级别胶质瘤的可能性。
术中:d,e,患者同意并在半坐位进行手术干预;在整个手术过程中持续监测经食管超声心动图,以早期发现可能的空气栓塞。我们进行了枕下正中大骨瓣开颅术,肿瘤通过四脑室经远外侧入路进入。根据术中菱形窝定位,肿瘤位于左侧面神经丘上方。由于肿瘤与周围的脑干实质有很好的区分,肿瘤被完全切除并在术后MRI上证实。
术后:术后运动功能完好,仅抱怨轻度的六神经麻痹引起轻微的半感觉障碍和轻微的复视。组织病理学检查为WHO1级毛细胞星形细胞瘤。患者术后未接受辅助治疗,症状逐渐缓解。她的后续康复良好。术后多次MRI检查均未发现局部肿瘤复发或其他颅内异常。f,术后11年随访,患者的临床状况良好,眼球运动正常,右手手指有轻微的非干扰性感觉缺陷。在11年的随访中,轴位(g)和矢状面(h)MRI显示患者没有肿瘤残留或复发。
This 20-year-old woman had extreme headache due to obstructive hydrocephalus caused by a large dorsally exophytic midbrain tumor. At first glance, preoperative axial (a,b) and sagittal (c) contrastenhanced magnetic resonance imaging (MRI) was suggestive of a highgrade tumor involving the midbrain and upper pons. However, as the patient had no neurologic deficits, tumor malignancy seemed rather unlikely, and the possibility of low-grade glioma was discussed with the patient and her family. We offered her direct surgery without initially treating the occlusive hydrocephalus. (d,e) The patient agreed and underwent the surgical intervention in the semisitting position; transesophageal echocardiography was continuously monitored throughout the procedure for early detection of possible air embolism. A large median suboccipital craniotomy was performed, and the tumor was accessed via the telovelar approach through the fourth ventricle. According to the intraoperative mapping of the rhomboid fossa, the tumor was located superior to the left facial colliculus. As the tumor was well distinguishable from the surrounding brainstem parenchyma, gross total tumor resection was achieved and confirmed on postoperative MRI. While the patient’s motor function was fully intact after surgery, she complained only of slight hemisensory disturbance and minimal diplopia caused by mild sixth nerve palsy. Histopathologic examination revealed a pilocytic astrocytoma World Health Organization grade I. The patient received no postoperative adjuvant therapy, and her symptoms gradually resolved. Her further clinical course was uneventful. Repeated postoperative MRIs documented the absence of local tumor recurrence or other intracranial abnormality. (f) Eleven years after surgery, the patient was in excellent clinical condition and had normal eye movement and only minimal, nondisturbing sensory deficits in the fingers of her right hand. Axial (g) and sagittal (h) MRIs at 11-year follow-up show that the patient remains free of tumor remnants or recurrence.
案例3:外生型顶盖乳头状胶质神经元瘤全切11年没有复发
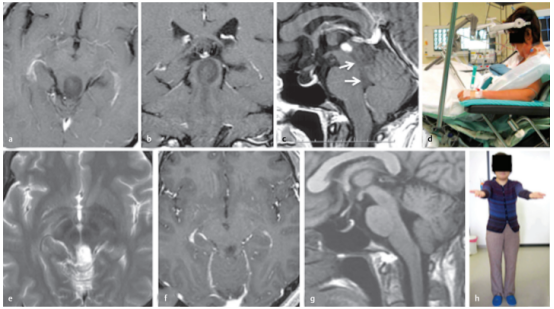
简要病史:36岁的女性因一个外生型顶盖肿瘤引起的闭塞性脑积水而出现严重头痛和步态共济失调。在另一家医院进行脑室腹腔分流术后症状消失。
术前:轴位(a)、冠状位(b)和矢状位(c)T1加权增强MRI显示肿瘤的确切位置及其尾端延伸至四脑室(c,箭头所示)。
术中:(d) 半坐位手术。肿瘤上半部分经幕下小脑上入路切除,其余下半部分经四脑室经前额叶暴露切除。组织病理学诊断为乳头状胶质神经元瘤。
术后:术后轴位(e)、冠状位(f)和矢状位(g)MRI显示肿瘤全切除。较后一次核磁共振是在手术后11年进行的;(h) 病人没有任何症状,过着独自的生活。
A 36-year-old woman had severe headache and gait ataxia due to occlusive hydrocephalus, which was caused by an exophytic tectal tumor. The symptoms disappeared after placement of a ventriculoperitoneal shunt in another hospital. Axial (a), coronal (b), and sagittal (c) T1-weighted contrast-enhanced magnetic resonance images (MRIs) demonstrate the exact tumor location and its caudal extension into the fourth ventricle (c, arrows). (d) The patient underwent surgery in the semisitting position. The superior tumor portion was resected via the supracerebellar infratentorial route, and the remaining inferior part via the telovelar exposure through the fourth ventricle in the same surgical procedure. Histopathologically, a papillary glioneuronal tumor was diagnosed. Postoperative axial (e), coronal (f), and sagittal (g) MRIs documented total tumor removal. The last MRI was performed 11 years after the surgical procedure. (h) The patient remained symptomfree and was leading an independent life.
脑干胶质瘤如何顺利手术?
术中神经电生理监测
脑干复杂的神经解剖组织,对神经外科医生来说是一个较大的挑战。在脑干内,脑神经核和上行、下行通路都在这里。肿瘤会扭曲脑干的正常解剖结构,比如四脑室底部的解剖标志,如面丘和髓质纹,使手术更具挑战性。术中神经生理监测和绘图的引入使手术更加顺利,并有助于制定手术计划,同时较大限度地降低对脑干关键结构的风险。
The complex neuroanatomic organization of the brain stem presents a formidable challenge to neurosurgeons when operating on lesions in this complex, small structure. Within the brain stem, cranial nerve nuclei and ascending and descending pathways are contained here. Tumors can distort the normal anatomy of the brain stem, such as anatomic landmarks on the floor of the fourth ventricle like the facial colliculus and striae medullares, and make surgery even more challenging. The introduction of intraoperative neurophysiologic monitoring and mapping has allowed for safer surgery and assisted in formulating the operative plan while minimizing risk to critical brain stem structures.
基于肿瘤的位置来使用神经电生理监测技术。可采取VII,IX/X和XII颅神经肌电监测。沿着四脑室底,脑桥和上延髓皮质切开前伴随低振幅单较刺激来示踪脑室底部,应该避免损伤面神经丘,以及迷走神经和舌下三角。
对于软膜下病变,较顺利的肿瘤暴露通道常常是选择肿瘤离皮层表面较近的部位,但也不总是这样选择。如果肿瘤累及到上下行纤维束,是颈延髓肿瘤,要采取体感诱发电位(SSEP)和运动诱发电位(MEP)监护。除了传统的外围电较放置,植入到手术床尾的硬膜外电较允许更快的更新运动诱发电位信号。
如果这些诱发电位振幅下降,其中MEP衰减是较可靠的提示。在信号下降的情况下,应停止切除,灌注术腔,避免任何对脑干/脊髓牵拉操作。如果电位恢复到基线水平,手术可能会继续;如果没有,进一步的干预会导致长期性神经功能缺损,因此需进行权衡。
此外,皮质脊髓束可以在脑脚的水平上进行定位,Kartush手持式刺激器(medtronicxomed,Inc.)通过对特定肌肉的肌电图监测,对中脑进行局部刺激。这种术中方式允许外科医生确定上述路径相对于肿瘤的位置,并顺利地在中脑切开。皮质脊髓束的定位有助于外科医生在病灶周围的解剖和活动中保护皮质脊髓束。
Moreover, the corticospinal tracts can be mapped at the level of the cerebral peduncles.A Kartush handheld stimulator (Medtronic Xomed, Inc.) is used to focally stimulate the midbrain with EMG monitoring of specific muscles. This intraoperative modality allows the surgeon to determine the location of the aforementioned pathways in relation to the tumor and safely make an incision in the midbrain. Localization of the corticospinal tracts assists the surgeon in an endeavor to protect them during the dissection around and mobilization of the lesion.
外科手术入路
脑干内肿瘤的位置和大小决定了外科医生的手术切除方法。在制定手术策略时,需考虑到脑干及其周围血管的复杂神经解剖结构。MRI被用来定位肿瘤,并计划较佳的路径到肿瘤,将损伤神经血管结构的风险降到较低。

图:显示到达脑干病变的相应手术入路。髓帆/枕下,乙状窦后,小脑上和眶颧手术入路适用于大多数病变。
对于脑桥背侧、四脑室底、延髓背侧和颈髓后交界处的肿瘤,我们倾向于患者俯卧位的枕下入路。小脑幕下入路可以到达顶盖中线区的肿瘤,我们也对俯卧位的患者进行此手术。后外侧桥、外侧小脑中脚、上外侧髓质和桥小脑角的病变可通过乙状窦后入路进入,远外侧入路提供脑干的前外侧路径,用于下外侧桥和前外侧髓质的病变。我们在乙状窦后入路和远外侧入路中都使用公园长椅位体位(park-bench position)。
For tumors in the dorsal pons, fourth ventricular floor, dorsal medulla, and posterior cervicomedullary junction, we prefer the suboccipital approach with the patient placed in the prone position. Tumors in the midline tectal region can be reached by the supracerebellar-infratentorial approach, and we also perform this procedure with the patient in the prone position. Lesions in the posterolateral pons, lateral middle cerebellar peduncle, superior lateral medulla, and cerebellopontine angle can be accessed through a retrosigmoid approach, and the far-lateral approach, which provides an anterolateral trajectory to the brain stem, is utilized for lesions in the inferolateral pons and anterolateral medulla. We use the park-bench position for both the retrosigmoid and far-lateral approaches.
颞下入路可进入中脑外侧病变。眶颧入路除中脑外侧外,还可进入桥嘴侧、脚间区和桥脑交界区。对于位于脑桥腹侧下部的病变,这些入路可结合前岩切除术。
The subtemporal approach provides access to lesions of the lateral midbrain. An orbitozygomatic approach provides additional access to the rostral pons, interpeduncular region, and pontomesencephalic junction in addition to the lateral midbrain. These approaches may be combined with an anterior petrosectomy for lesions located more inferior in the ventral pons.
外科技术
脑干复杂的神经解剖结构在切除肿瘤时需要仔细的显微外科技术。小小的脑干要求精确的运动和良好的术中判断。一个功能较佳的手术显微镜对脑干内部和周围的手术至关重要。内生性肿瘤需要在脑干表面开一个切口,并需要对解剖学有透彻的了解。虽然许多肿瘤可以在较接近表面的地方进行探查,但需记住,在某些情况下,这可能不是较佳途径。切口通常小于1cm,为切除大肿瘤提供了足够的空间。脑干皮层脊髓束附近的肿瘤可以被定位为一个顺利的切入点。对于经由四脑室底入路的肿瘤,对四脑室底的定位对于切口的放置重要,以避免颅神经核,如VII、IX、X和XII。此外,有些脑干区域可以相对顺利地进入。经四脑室底入路的脑桥背肿瘤可经面丘上方正中沟、面表面、面下及听神经区进入。顶盖中脑肿瘤可经滤泡上、滤泡下和外侧中脑沟进入,而髓质和颈髓肿瘤可在obex下的后正中裂、后中沟和后外侧沟行纵向脊髓切开术。
The complex neuroanatomic structure of the brain stem requires very careful microsurgical technique when resecting tumors. The small dimensions of the brain stem demand precise movements and good intraoperative judgment at all times. An optimally functioning surgical microscope is vital to operations in and around the brain stem.Intrinsic tumors necessitate an incision in the surface of the brain stem and require a thorough understanding of the anatomy. Although many tumors can be accessed where it is closest to the surface, it must bear in mind that this may not be the optimal route in some cases. The incision is usually small and less than 1 cm, which typically provides enough space for the resection of large tumors. Tumors in the vicinity of the corticospinal tracts in the cerebral peduncles can be mapped for a safe entry point. For tumors approached through the fourth ventricular floor, mapping of the floor is extremely important for placement of the incision to avoid cranial nerve nuclei, such as VII, IX, X, and XII. In addition, there are areas of the brain stem that can be entered relatively safely. Dorsal pontine tumors approached through the fourth ventricular floor can be entered through the median sulcus above the facial colliculus, suprafacial, infrafacial, and area acoustica. Tectal mesencephalic tumors can be accessed through the supracollicular, infracollicular, and lateral mesencephalic sulcus, while longitudinal myelotomies can be performed in the posterior median fissure below the obex, posterior intermediate sulcus, and posterior lateral sulcus for medullary and cervicomedullary tumors.
一旦到达肿瘤,它的一致性将被评估,并将根据外科医生的喜好决定切除的方法。肿瘤标本应尽快提交,以确定组织学。组织学将决定是否可行全切除,这在良性肿瘤的情况下更有可能。根据外科医生的喜好,可以使用微牵开器。肿瘤应该一点一点地切除,而不是整块整块地切除。如果囊肿与肿瘤相关,切除囊性液体可以提供额外的操作空间,从而有助于肿瘤的减容。低强度、低吸引率的超声吸引和/或显微手术对实体瘤更合适。微双较凝血术和同时抽吸凝血组织可用于软组织肿瘤。手术切除需局限于肿瘤内部,以避免损伤周围正常结构。在大部分肿瘤去瘤后,寻找肿瘤和正常脑之间的正常边界。当肿瘤和正常脑之间的界限被确定时,在大多数情况下全切除是可行的。当无法看到两者之间的界面时,应停止肿瘤切除,因为决定继续对病灶进行减厚可能会增加术后神经系统并发症的机会。此外,一些肿瘤可能具有高血管密度,在肿瘤减容时血管需凝固,这可能会对周围正常大脑造成缺血性损伤。
Once the tumor has been reached, its consistency is evaluated and will determine the method of extirpation according to the surgeon’s preference. A tumor specimen should be submitted as soon as possible for determination of the histology. The histology will determine if a gross-total resection is feasible, which is more likely in the case of benign tumors. Depending on the surgeon’s preference, microretractors may be used. Tumors should be removed in a piecemeal fashion and not en bloc. If a cyst is associated with the tumor, removal of the cystic fluid aids in tumor debulking by providing additional space for manipulation. Ultrasonic aspiration set at a low intensity and suction rate and/or microscissors are more effective for solid tumors. Microbipolar coagulation and simultaneous aspiration of coagulated tissue may be used for soft tumors. The surgical resection must be confined to the inside of the tumor to avoid injury to normal surrounding structures. After a majority of the tumor is debulked, a normal boundary between the tumor and normal brain is sought. When delineation between tumor and normal brain is identified, gross-total resection is feasible in most cases. Tumor resection should be stopped when an interface between the two cannot be visualized because the decision to continue with debulking the lesion may increase the chances of postoperative neurologic morbidity. In addition, some tumors may be highly vascular and the vessels must be coagulated during tumor debulking, which may cause ischemic damage to surrounding normal brain.
对于具有外生成分的局灶性肿瘤,肿瘤的这一突出部分提供了手术进入肿瘤的途径。此外,穿透蛛网膜下腔的肿瘤可能接触或包裹重要动脉,而穿透脑干腹侧的肿瘤可能接触椎动脉或基底动脉及其分支;因此,需小心地处理这些肿瘤。起源于脑桥或髓质室管膜下的肿瘤,没有或很少侵犯脑干,并突出到四脑室,是良性背侧外生肿瘤的一个亚组,可以成功切除。
For focal tumors with an exophytic component, this protruding aspect of the tumor provides an avenue for surgical access to the tumor. Moreover, tumors that penetrate the subarachnoid space may contact or encase vital arteries, and those that penetrate the ventral brain stem may contact
the vertebral or basilar arteries and their branches; therefore, these tumors must be approached with extreme caution. Tumors arising from the subependymal aspect of the pons or medulla with no or minimal brain stem invasion and protruding into the fourth ventricle comprise a subgroup of dorsally exophytic tumors that are benign and can be resected with success.
后记
脑干手术对神经外科医生来说是一个较大的挑战,但影像学、手术方法和术中神经生理监测的进步降低了与这些手术相关的风险和发病率。有或无外生成分的局灶性内生脑干肿瘤和原发性外生病变均需手术切除( Focal intrinsic brain stem tumors with or without an exophytic component and primarily exophytic lesions are indicated and amenable to surgical resection. )。尽管脑干手术的显微外科技术已经取得了进展,但这些技术的持续发展仍需要为患者提供尽可能好的护理,致力提高患者的生活质量。
INC旗下国际神经外科顾问团是由国际各发达国家神经外科宗师联合组成的教授集团,其成员教授大多为国际神经外科各的奠基者、开拓者,德国巴特朗菲教授即为成员教授之一,曾接诊过多例国内及国际各地的脑干、丘脑、基底节区、胼胝体等复杂位置脑瘤患者,在国内,他被患者亲切称为“巴教授”。巴教授专注脑干、颅底等复杂手术30多年、上千台成功脑干手术记录:包括800台脑干胶质瘤成功案例、300台脑干海绵状血管瘤成功案例等,大部分脑干肿瘤手术患者,术后ICU观察一天,气管插管不超过1天,术后少有肢体瘫痪、颅神经损伤急需呼吸机支持、长期卧床的患者,这无疑是成功的高难度手术较直接合适的证明。除了脑干,其他神经外科疑难的位置,如颅底、功能区、颅颈交界处、脊髓等也拥有众多成功手术病例,近几年他还为中国的患者进行了多台成功的疑难手术。
参考资料:1.Helmut Bertalanffy. Chapter 13 Adult Brainstem Gliomas. Surgery of the Brainstem.Thime. 2020.
2.JAMES L. FRAZIER.GEORGE I. JALLO.CHAPTER 13 Schmidek and Sweets Operative Neurosurgical Techniques .Surgical Management of Brain Stem Tumors in Adults
3.DOI: https://doi.org/10.18791/nsatlas.v4.ch03.1
- 文章标题:面对脑干胶质瘤束手无策?顺利全切后10年以上没有复发案例3则
- 更新时间:2021-01-12 14:30:06

 400-029-0925
400-029-0925