Abstract
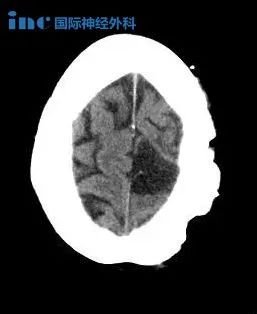
Objective:The object of this study was to investigate the impact of facility type(academic center[AC]vs non-AC)and facility volume(high-volume facility[HVF]vs low-volume facility[LVF])on low-grade glioma(LGG)outcomes.
Methods:This retrospective cohort study included 5539 LGG patients(2004-2014)from the National Cancer Database.Patients were categorized by facility type and volume(non-AC vs AC,HVF vs LVF).An HVF was defined as the top 1%of facilities according to the number of annual cases.Outcomes included overall survival,treatment receipt,and postoperative outcomes.Kaplan-Meier and Cox proportional-hazards models were applied.The Heller explained relative risk was computed to assess the relative importance of each survival predictor.
Results:Significant survival advantages were observed at HVFs(HR 0.67,95%CI 0.55-0.82,p<0.001)and ACs(HR 0.84,95%CI 0.73-0.97,p=0.015),both prior to and after adjusting for all covariates.Tumor resection was 41%and 26%more likely to be performed at HVFs vs LVFs and ACs vs non-ACs,respectively.Chemotherapy was 40%and 88%more frequently to be utilized at HVFs vs LVFs and ACs vs non-ACs,respectively.Prolonged length of stay(LOS)was decreased by 42%and 24%at HVFs and ACs,respectively.After tumor histology,tumor pattern,and codeletion of 1p19q,facility type and surgical procedure were the most important contributors to survival variance.The main findings remained consistent using propensity score matching and multiple imputation.
Conclusions:This study provides evidence of survival benefits among LGG patients treated at HVFs and ACs.An increased likelihood of undergoing resections,receiving adjuvant therapies,having shorter LOSs,and the multidisciplinary environment typically found at ACs and HVFs are important contributors to the authors'finding.
目的:探讨设施类型(学术中心与非中心)和设施容量(高容量设施与低容量设施)对低级别胶质瘤(LGG)预后的影响。
方法:这项回顾性研究包括来自国家癌症数据库的5539例LGG患者(2004-2014)。根据设备类型和容量(非AC vs AC,HVF vs LVF)对患者进行分类。根据年度案例的数量,HVF被定义为设施的前1%。结果包括总生存率、接受治疗和术后结果。应用Kaplan-Meier和Cox比例风险模型。计算相对风险是为了评估每个生存评估因子的相对重要性。
结果:在校正全部协变量之前和之后,HVFs(HR 0.67,95%CI 0.55-0.82,p<0.001)和ACs(HR 0.84,95%CI 0.73-0.97,p=0.015)观察到的生存优势。在HVFs组、LVFs组和ACs组与非ACs组相比,肿瘤切除率分别高41%和26%。在lvacs中使用率分别为88%和88%。HVFs组和ACs组延长住院时间(LOS)分别减少42%和24%。在肿瘤组织学、瘤种和1p19q编码后,设备类型和手术方式是影响存活率的较重要因素。使用倾向评分匹配和多重插补,主要结果保持一致。
结论:本研究为在HVFs和ACs治疗的LGG患者提供了生存益处的证据。手术切除的可能性增加,接受辅助治疗,LOSs更短,以及在ACs和HVFs典型的多学科环境是作者发现的重要因素。
关于美国Mitchel Berger教授

Mitchel Berger教授来自美国神经外科医院三、国际闻名的神经外科疾病研究和治疗机构UCSF医学中心。Mitchel Berger教授是全美公认的成人及儿童脑肿瘤治疗专家,在任职UCSF神经外科主席之前,他还担任过美国神经外科协会主席、美国神经学医师协会主席、美国癌症研究协会州立法委员会主席、北太平洋神经及神经外科和精神病学会主席,在神经外科疾病临床咨询、癌症研究和基因治疗等方面有突出贡献。目前,Mitchel Berger教授是UCSF医学中心SPORE脑肿瘤项目的研究员,也是美国国家“癌症登月”计划蓝带小组专家。
除了在美国享誉盛名,Mitchel Berger教授更是神经外科领域内清醒开颅手术、脑功能监测技术方面的专家,在脑部术中建图方面拥有丰富的知识,能够准确识别运动、感觉和语言功能的部位,从而避免在手术过程中伤及重要神经,能在很大水平上保障手术的准确性和顺利性。由Mitchel Berger教授发明的超声引导手术器械方法获得了美国专利商标局(USPTO)授予的专利,目前已在神经外科领域广泛推广使用。
原文链接:https://www.sci-hub.pl/https://thejns.org/view/journals/j-neurosurg/aop/article-10.3171-2019.6.JNS19409.xml
- 文章标题:INC美国Mitchel Berger教授:低级别胶质瘤预后的影响因素
- 更新时间:2020-08-10 14:41:41

 400-029-0925
400-029-0925